Free Testosterone Matters More Than Total—But Your Lab Might Be Calculating It Wrong
Published on:
Updated on:
People are asking...
Your 'expert' Finasteride video: https://www.youtube.com/watch?v=mKum5L64cPk @ 2:07 Your 'expert' dudebro says serum DHT concentrations were 100 time...
He did misspeak, thank you for pointing that out. Yes, DRUG concentrations were >100 less with the topical vs the oral version of finasteride. As always, our YouTube channel is an informal venue, and ... See Full Answer
Would a person that has low test and takes trt build more or less muscle than an average person that doesn’t take anything?...
They would generally build the same amount of muscle, assuming that "average person" was not also a low Testosterone individual. This is because the primary goal of TRT is to get you back to where you... See Full Answer
I've been on TRT for 1.5 years and have not been able to figure out why it has caused ED. Estrogen is where it should be. I'm not on excess T. Not on ...
The melanocortin receptor pathway is a relatively newly discovered mechanism for both erectile function and libido. It is entirely separate from traditional hormonal pathways previously thought to be ... See Full Answer
Have a question? Ask us.
At AlphaMD, we're here to help. Feel free to ask us any question you would like about TRT, medical weightloss, ED, or other topics related to men's health. Or take a moment to browse through our past questions.
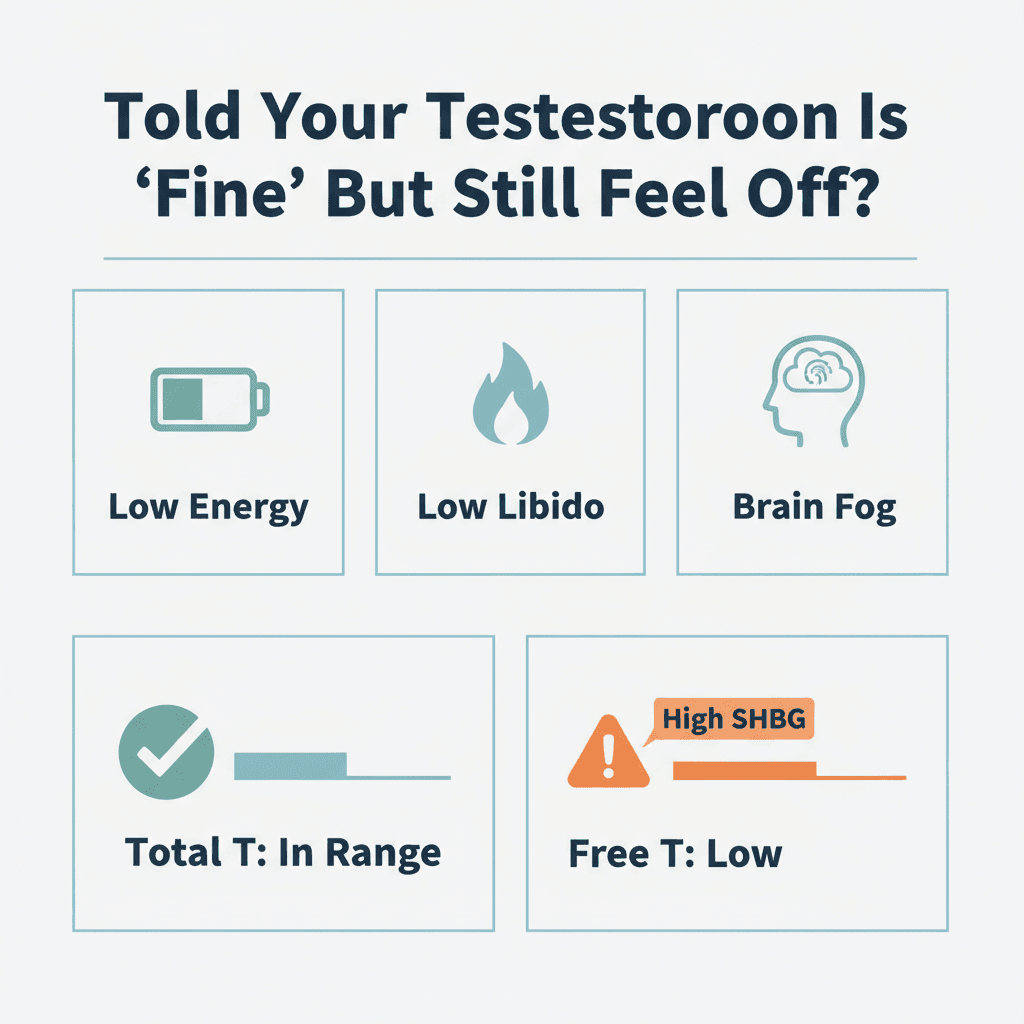
You're tired, your libido has disappeared, you're putting on belly fat despite eating the same way you always have, and your brain feels like it's wrapped in fog. But your doctor just told you your testosterone is "fine," handed you a printout with a number in the reference range, and suggested you sleep more or maybe see a therapist. If this sounds familiar, the problem might not be that your testosterone is normal - it's that your lab is only telling half the story, and possibly calculating the most important half incorrectly.
The testosterone number your doctor quoted is almost certainly your total testosterone, which measures all the testosterone floating around in your bloodstream. But most of that testosterone is locked up, bound tightly to proteins and unavailable for your body to actually use. What matters for how you feel, how you perform, and how your body functions is free testosterone - the small fraction that's unbound and biologically active. And when labs estimate free testosterone using outdated formulas or incomplete data, they can make a low level look normal, or miss a problem entirely.
Why Most of Your Testosterone Is Parked, Not Driving
Think of total testosterone like all the cars in a parking lot. Free testosterone is the much smaller number of cars actually on the road with keys in the ignition, doing the work of getting people where they need to go.
In your bloodstream, roughly 98% of testosterone is bound to proteins - primarily sex hormone binding globulin (SHBG) and albumin. SHBG holds testosterone very tightly, essentially taking it out of circulation. Albumin binds testosterone more loosely, and some of that testosterone can dissociate and become active. But the truly free, unbound testosterone - the portion that can cross into cells and bind to androgen receptors in your muscles, brain, bones, and sexual tissues - makes up only about 2-3% of your total.
That small percentage does the heavy lifting. Free testosterone is what triggers protein synthesis in muscle tissue, supports cognitive function and mood, drives libido and sexual function, influences fat distribution, and maintains bone density. When free testosterone is low, you feel it, even if your total testosterone number looks perfectly acceptable on paper.
When "Normal" Total Testosterone Hides a Real Problem
This is where the disconnect happens for many men. Your total testosterone might sit comfortably in the middle of the reference range, but if your SHBG is elevated, more of that testosterone is bound up and unavailable. The result? Low free testosterone and all the symptoms that come with it.
Several factors can drive SHBG higher and reduce free testosterone availability:
Age is a major player. As men get older, SHBG levels tend to rise, even as total testosterone gradually declines. This double effect can leave free testosterone particularly low in middle-aged and older men.
Excess body fat, especially visceral fat around the organs, creates a hormonal environment that can affect the balance between testosterone, estrogen, and binding proteins. More body fat often means less free testosterone available to do its job.
Thyroid disorders, particularly hyperthyroidism, can elevate SHBG. Even subclinical thyroid issues can shift the balance.
Certain medications, including some used for epilepsy, HIV, and other chronic conditions, can increase SHBG and reduce free testosterone.
Genetics matter too. Some men naturally produce more SHBG than others, which means they need higher total testosterone levels just to maintain adequate free testosterone.
The key insight is this: a man with moderate total testosterone but high SHBG can have worse symptoms and lower free testosterone than a man with slightly lower total testosterone but normal SHBG. The total number alone does not tell you what your body actually has access to.
Your Lab Probably Isn't Measuring Free Testosterone - It's Guessing
When you get a testosterone panel, most commercial labs do not directly measure your free testosterone. Instead, they calculate it using a formula based on your total testosterone, SHBG, and sometimes albumin levels.
This matters because calculated free testosterone is only as good as the formula being used and the accuracy of the input values. Different labs use different equations. Some use older formulas that have been shown to be less accurate. Others use more modern calculations that better account for binding dynamics, but even these have limitations and can vary between platforms.
Small measurement errors in SHBG or albumin can get amplified when plugged into a formula, leading to calculated free testosterone values that are significantly off from what a direct measurement would show. And because reference ranges for free testosterone also vary widely between labs, the same blood sample analyzed at two different facilities can yield two different interpretations - one saying you're normal, the other suggesting a problem.
Imagine a scenario where a man feels all the classic symptoms of low testosterone. His total testosterone comes back in the normal range, so his doctor says everything looks fine. But his SHBG was on the high side, which the doctor didn't pay much attention to. The lab's calculated free testosterone also showed up in the reference range, but the formula used was conservative and the SHBG measurement had some variability. A more precise assessment using a better calculation method or a direct measurement technique would have revealed that his free testosterone was actually quite low, explaining his symptoms perfectly. Instead, he's told to exercise more and deal with it.
This is not a hypothetical edge case. It happens regularly.
Direct Measurement vs Calculation: Why the Method Matters
Directly measuring free testosterone is technically challenging and expensive. Methods like equilibrium dialysis and ultrafiltration are considered more accurate but are usually reserved for research settings or specialized labs. Most routine clinical labs rely on immunoassays or calculated values because they're faster and cheaper.
Some professional medical societies have endorsed specific calculation methods, like the Vermeulen equation, as reasonable alternatives when direct measurement isn't available. These calculations are certainly better than ignoring free testosterone altogether, but they're still estimates, and estimates can be wrong.
The clinical reality is that free testosterone is often treated as an afterthought. Many doctors focus almost exclusively on total testosterone because that's what they were taught, because it's easier to interpret, or because they simply aren't aware of the nuances. But for men with symptoms, especially those with borderline total testosterone or risk factors for high SHBG, looking only at total testosterone can mean missing a very real problem.
Context is everything. One free testosterone number, especially if it's calculated rather than measured, should never be the sole basis for a decision. It needs to be considered alongside total testosterone, SHBG, symptoms, medical history, and overall health.
The Symptoms Your Lab Values Should Explain
Lab ranges are built from population data - they reflect what's statistically normal across large groups of men, including men of different ages and health states. But normal for a population is not the same as optimal for you as an individual.
Low free testosterone tends to produce a recognizable pattern of symptoms:
Energy and motivation take a hit. You feel tired even after a full night's sleep. Tasks that used to be easy feel like they require monumental effort. You find yourself dragging through the day.
Sex drive and function decline. Libido drops, erections become less reliable, and the whole domain of sexual health feels diminished.
Body composition shifts. Building or maintaining muscle becomes harder despite training. Fat, particularly around the midsection, accumulates more easily. You look softer even if your weight hasn't changed much.
Mood and cognition suffer. You might feel lower mood, increased irritability, or a general sense of flatness. Brain fog, poor concentration, and memory issues can creep in.
Sleep quality often worsens, creating a vicious cycle since poor sleep further disrupts hormone production.
If you're experiencing several of these symptoms persistently, and your doctor has only looked at total testosterone, you're not getting the full picture. This is when you need to ask better questions.
Questions to Ask Your Doctor About Your Testosterone Labs
Advocating for yourself in a healthcare setting can feel uncomfortable, but it's necessary, especially when symptoms and lab values don't seem to match. Come prepared with specific questions:
"Are you looking at both my total and free testosterone, and how is my free testosterone being determined?" This gets directly at whether free testosterone is even part of the evaluation and whether it's measured or calculated.
"What is my SHBG level, and how does that affect my free testosterone?" This shows you understand the binding protein issue and want a more nuanced interpretation.
"Do my symptoms align with my lab values, or is there a mismatch we should investigate further?" This frames the conversation around your actual experience, not just numbers on a page.
"If my total testosterone is normal but I have symptoms, could my free testosterone be low?" This directly challenges the idea that a normal total testosterone means everything is fine.
"Would it make sense to retest using a different method or look at additional markers?" This opens the door to more thorough testing if the initial results don't make sense.
You're not questioning your doctor's competence - you're asking for a more complete evaluation. Any good clinician will appreciate a patient who is engaged and informed.
Testosterone Replacement Therapy: When and How Clinicians Decide
When testosterone replacement therapy is considered, the decision should involve much more than a single total testosterone measurement. Thoughtful clinicians look at the whole picture: total testosterone, free testosterone, SHBG, symptoms, medical history, age, lifestyle factors, and overall health goals.
TRT is not a one-size-fits-all intervention. It's a medical treatment with real benefits when indicated and real risks when misused or poorly monitored. The goal is to restore testosterone levels to a range that alleviates symptoms and supports health, while monitoring for potential side effects like changes in red blood cell count, prostate health markers, cardiovascular effects, and fertility impact.
Before jumping to TRT, many clinicians also address modifiable factors that affect testosterone production and availability. Sleep is foundational - chronic sleep deprivation suppresses testosterone production. Body composition matters - losing excess fat, particularly visceral fat, can improve free testosterone by reducing SHBG and aromatase activity. Nutrition plays a role, as severe calorie restriction or nutrient deficiencies can tank hormone levels. Alcohol consumption can suppress testosterone production and increase estrogen. Resistance training supports healthy testosterone levels and improves body composition.
Addressing these factors won't fix primary hypogonadism, but they can make a meaningful difference for men whose testosterone has declined due to lifestyle and metabolic issues. And when TRT is appropriate, optimizing these factors alongside treatment improves outcomes.
The critical point is that TRT decisions should be individualized and based on both biochemistry and symptoms, not a checkbox based solely on whether total testosterone falls below an arbitrary cutoff.
A Different Approach: How Modern Men's Health Services Are Changing the Conversation
Traditional primary care is often constrained by time, outdated protocols, and limited familiarity with nuanced hormone management. A fifteen-minute appointment doesn't leave much room to discuss the difference between total and free testosterone, interpret SHBG, or explore why symptoms don't match lab values.
This is where specialized men's health services like AlphaMD have found their niche. AlphaMD is an online platform focused specifically on men's health and testosterone replacement therapy, and it takes a more thorough approach to hormone evaluation. Rather than relying on a single total testosterone number and a quick reference range check, AlphaMD clinicians consider free testosterone, SHBG, symptoms, and the broader health context when assessing whether treatment makes sense.
For men who have been told their testosterone is "fine" despite feeling decidedly not fine, this kind of service offers a second look from clinicians who specialize in exactly this issue. The process is designed to be accessible - consultations happen online, labs can be ordered conveniently, and treatment plans are tailored to the individual rather than following a rigid protocol.
AlphaMD isn't the only option in this space, but it represents a shift toward more patient-centered, symptom-aware hormone care. The model acknowledges that reference ranges are guidelines, not gospel, and that how a man feels matters just as much as what his labs say.
What This Means for Your Hormone Health
The central message is simple but powerful: free testosterone often matters more than total testosterone for understanding symptoms, and how your lab calculates free testosterone can dramatically affect whether a problem gets identified or dismissed.
If you're experiencing low energy, reduced sex drive, difficulty building muscle, increased body fat, poor sleep, low mood, or brain fog, and you've been told your testosterone is normal, don't accept that answer without digging deeper. Ask about free testosterone. Ask about SHBG. Ask how free testosterone was determined and whether your symptoms match your lab values.
You deserve care that takes your experience seriously and looks beyond a single number on a standard lab panel. Whether that comes from your current doctor, a specialist, or a service like AlphaMD that focuses on hormone optimization, the key is finding a clinician who understands the nuances and is willing to investigate when symptoms and labs don't align.
Better testing leads to better explanations, and better explanations lead to better treatment decisions. Your hormones are complex, and your health deserves a more sophisticated approach than a glance at total testosterone and a pat on the back. Services like AlphaMD are designed to provide exactly that - more complete testing, clearer interpretation, and treatment plans that actually match what's happening in your body.
If your labs say you're fine but your body is telling you something different, trust your body and ask better questions. The right answers are out there, and they start with looking at free testosterone the right way.
Have a question? Ask us.
At AlphaMD, we're here to help. Feel free to ask us any question you would like about TRT, medical weightloss, ED, or other topics related to men's health. Or take a moment to browse through our past questions.
People are asking...
Your 'expert' Finasteride video: https://www.youtube.com/watch?v=mKum5L64cPk @ 2:07 Your 'expert' dudebro says serum DHT concentrations were 100 time...
He did misspeak, thank you for pointing that out. Yes, DRUG concentrations were >100 less with the topical vs the oral version of finasteride. As always, our YouTube channel is an informal venue, and ... See Full Answer
Would a person that has low test and takes trt build more or less muscle than an average person that doesn’t take anything?...
They would generally build the same amount of muscle, assuming that "average person" was not also a low Testosterone individual. This is because the primary goal of TRT is to get you back to where you... See Full Answer
I've been on TRT for 1.5 years and have not been able to figure out why it has caused ED. Estrogen is where it should be. I'm not on excess T. Not on ...
The melanocortin receptor pathway is a relatively newly discovered mechanism for both erectile function and libido. It is entirely separate from traditional hormonal pathways previously thought to be ... See Full Answer
Get $30 off your first month’s order
Enter your email address now to receive $30 off your first month’s cost, other discounts, and additional information about TRT.
Legal Disclaimer
This website is a repository of publicly available information and is not intended to form a physician-patient relationship with any individual. The content of this website is for informational purposes only. The information presented on this website is not intended to take the place of your personal physician's advice and is not intended to diagnose, treat, cure, or prevent any disease. Discuss this information with your own physician or healthcare provider to determine what is right for you. All information is intended for your general knowledge only and is not a substitute for medical advice or treatment for specific medical conditions. The information contained herein is presented in summary form only and intended to provide broad consumer understanding and knowledge. The information should not be considered complete and should not be used in place of a visit, phone or telemedicine call, consultation or advice of your physician or other healthcare provider. Only a qualified physician in your state can determine if you qualify for and should undertake treatment.
