6 TRT Myths Your Doctor STILL Believes in 2026 (And Why They're Dead Wrong)
Published on:
Updated on:
People are asking...
I'm a 36-year-old male, I've been on TRT for hypogonadism for about 10 years now. The TRT specialist/internist I was getting treatment with, emigrate...
We hear a story like yours all the time. GP’s have a lot of things they have to keep up on. New treatments for diabetes, new diagnostics for rheumatic conditions, new screening rules for breast cance... See Full Answer
Age 62, athletic, nutrition freak (usa). Started TRT 15 months ago when testosterone at 298. Six months later it was 498 and I was doing great. Level ...
I'll share some conjecture here without knowing more. Taking everything at face value, I would say whatever medication you're taking might not be Testosterone Cypionate. When you take any Testosterone... See Full Answer
Hi, I’m 25 years old. Test is 404. I work out 5 days per week, am pretty lean and fit and healthy I had previously considered TRT but ultimately turn...
A few things to note: You may have relative hypogonadism where your numbers just being low aren't the main factor to determine treatment. 400 would be within that range. You will lose Testosterone ove... See Full Answer
Have a question? Ask us.
At AlphaMD, we're here to help. Feel free to ask us any question you would like about TRT, medical weightloss, ED, or other topics related to men's health. Or take a moment to browse through our past questions.
Your doctor just told you your testosterone levels are "fine" and sent you home with a prescription for an antidepressant. Meanwhile, you can barely drag yourself out of bed, your libido is non-existent, and you're wondering if this is just what getting older feels like.
The truth is, you might be caught in the middle of a medical knowledge gap that's leaving thousands of men undertreated and overworked. Despite mounting evidence and evolving clinical guidelines, many physicians still cling to outdated beliefs about testosterone replacement therapy that were formed decades ago. These myths aren't just wrong, they're actively preventing men from getting the evaluation and care they deserve.
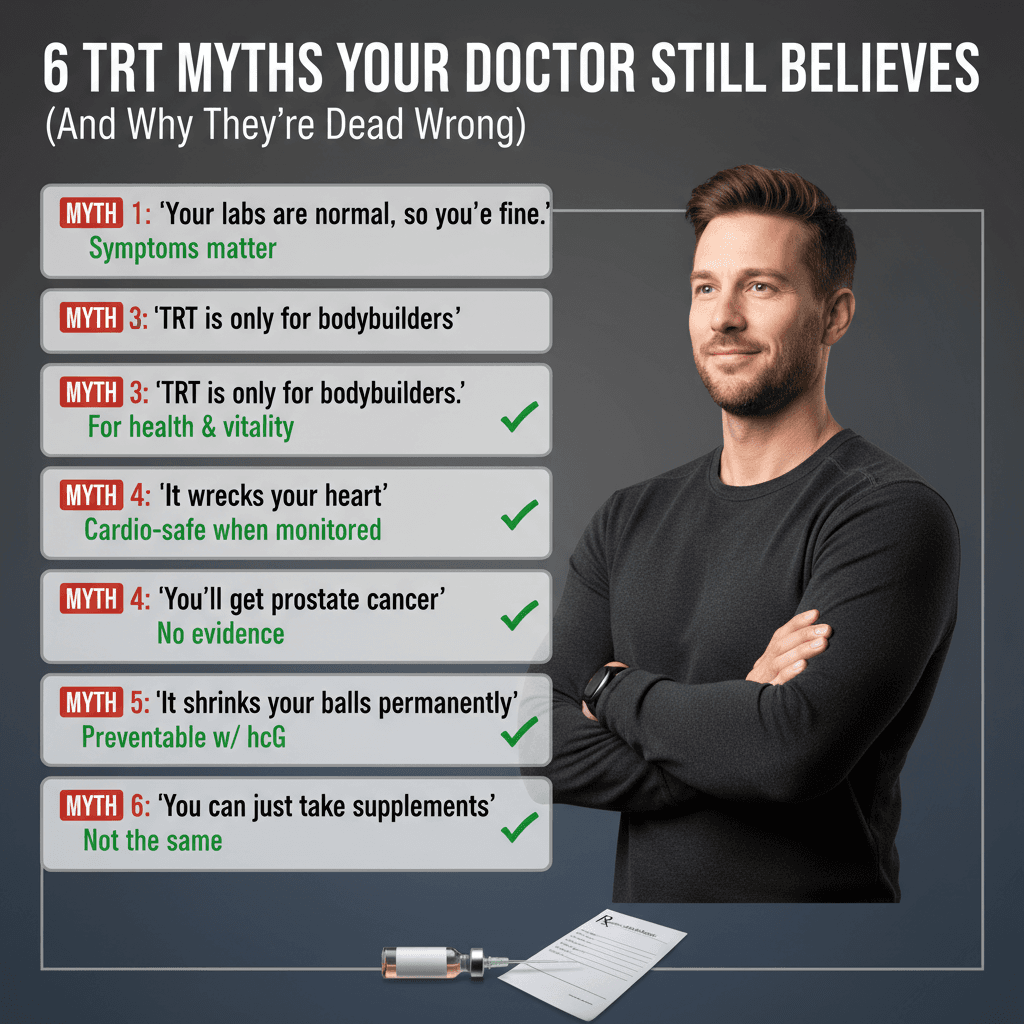
Let's examine six of the most persistent TRT misconceptions that continue to circulate in medical offices across the country, and why the science tells a very different story.
Why "Normal" Labs Still Leave You Feeling Half-Alive
You've heard it before: your testosterone came back within the reference range, so there's nothing wrong with you. Case closed.
Except that reference ranges for testosterone are notoriously broad, often encompassing values that might be appropriate for an 80-year-old man but catastrophically low for someone in their 30s or 40s. These ranges are typically generated from population samples that include men of all ages, health conditions, and baseline hormonal profiles. Being "in range" tells you almost nothing about whether your testosterone level is optimal for you as an individual.
Many physicians were trained to treat lab values rather than patients. If the number falls between the lines on the report, they assume everything is fine. This approach ignores the reality that hormone optimization is highly individual. Some men feel fantastic at the lower end of normal, while others experience debilitating symptoms despite being technically within range.
Modern hormone medicine recognizes that symptoms matter just as much as lab values, if not more. A man presenting with classic signs of low testosterone (persistent fatigue, mood changes, reduced muscle mass, diminished sexual function, brain fog) deserves a thorough evaluation and treatment consideration even if his numbers aren't in the basement. The goal isn't to hit an arbitrary lab target, it's to restore quality of life while maintaining safety.
This myth persists because it's simpler to follow algorithmic care based on reference ranges than to practice individualized medicine. But simple isn't always right.
The Prostate Cancer Scare That Won't Die
For decades, testosterone was treated as fuel for prostate cancer, a dangerous substance that would inevitably lead to malignancy if replaced therapeutically. This belief has been so deeply ingrained that many doctors still reflexively warn patients that TRT will damage their prostate or cause cancer.
The origin of this myth traces back to a single 1941 study showing that castration could slow advanced prostate cancer. The logic seemed straightforward: if removing testosterone helped treat existing cancer, then adding testosterone must cause it. But correlation is not causation, and medicine has learned a great deal in the eight decades since.
Current evidence does not support the claim that testosterone replacement causes prostate cancer in men without pre-existing malignancy. Multiple large studies and meta-analyses have failed to demonstrate an increased risk of prostate cancer in men receiving properly monitored TRT. In fact, some research suggests that men with low testosterone may actually have more aggressive prostate cancers when they do develop.
What testosterone can do is accelerate the growth of existing hormone-sensitive prostate cancers. This is why appropriate screening before starting TRT and regular monitoring during treatment are essential. Men with known prostate cancer or significantly elevated prostate-specific markers are generally not candidates for TRT. But for men without these contraindications, the data simply doesn't support the fear-driven approach many doctors still take.
This myth has done tremendous harm by scaring both physicians and patients away from a therapy that could significantly improve quality of life. Fear is a poor substitute for evidence-informed care.
The Heart Attack Myth That Keeps Getting Repeated
If the prostate cancer myth is the oldest, the cardiovascular risk myth might be the most controversial. You've probably heard that TRT causes heart attacks, increases stroke risk, or generally threatens cardiovascular health. Some doctors still cite this as a primary reason to avoid testosterone therapy altogether.
This myth gained traction after several studies in the early 2010s suggested potential cardiovascular risks. These studies had significant methodological flaws, including biased patient selection, inadequate follow-up periods, and failure to control for confounding variables. Yet they generated alarming headlines that many clinicians still remember.
Subsequent, more rigorous research has painted a very different picture. Large, well-designed studies have shown that properly administered TRT does not increase cardiovascular risk in appropriate candidates, and may actually be cardioprotective in some populations. Low testosterone itself is associated with increased cardiovascular disease, metabolic syndrome, and overall mortality.
The nuance that often gets lost is that TRT, like any medical intervention, requires appropriate patient selection and monitoring. Men with uncontrolled heart disease, recent cardiovascular events, or certain other risk factors may not be suitable candidates, at least initially. But for otherwise healthy men with genuine testosterone deficiency, the cardiovascular data is largely reassuring.
What's particularly frustrating about this myth is that it often leads doctors to withhold potentially beneficial treatment from men who are already at cardiovascular risk due to obesity, metabolic dysfunction, and low testosterone itself. The decision shouldn't be driven by outdated fear, but by careful assessment of individual risk factors and potential benefits.
The Permanent Shutdown Fallacy
One of the most anxiety-inducing myths men hear is that starting TRT means permanently shutting down their natural testosterone production, leaving them dependent on injections or gels for life with no possibility of recovery.
There's a kernel of truth here that gets wildly distorted. When you introduce exogenous testosterone, your body's feedback system detects adequate hormone levels and reduces its own production. For many men on TRT, natural production does decrease significantly or stop altogether during treatment. This is expected and not inherently harmful.
But "shutdown" doesn't mean "destroyed." In many cases, if TRT is discontinued, the body's natural production can recover, especially with appropriate medical management. Recovery protocols using medications that stimulate natural testosterone production have helped many men successfully discontinue TRT when desired or necessary. Success rates vary based on factors like age, duration of treatment, and baseline function, but the idea that starting TRT means permanent, irreversible dependency is simply false.
That said, some men may find that their natural production doesn't fully recover, particularly if they were already borderline or deficient before starting treatment, or if they're older when they attempt to stop. And many men who feel significantly better on TRT have no desire to discontinue it, which is a perfectly reasonable choice.
The important point is that starting TRT should be an informed decision made with full understanding of how it works, but it shouldn't be avoided purely out of fear that you're flipping an irreversible switch. Medicine is rarely that black and white.
The Vanity Drug Dismissal That Minimizes Real Suffering
Perhaps no myth is more dismissive and damaging than the belief that TRT is merely a vanity treatment for aging men who can't accept getting older, or worse, a performance-enhancing drug for bodybuilders masquerading as medicine.
This perspective reveals a profound misunderstanding of what testosterone deficiency actually does to men's lives. Low testosterone isn't about having slightly less muscle definition or reduced gym performance. It's about debilitating fatigue that makes basic daily functioning difficult. It's about depression and anxiety that don't respond to conventional treatment. It's about loss of cognitive sharpness, motivation, and the essential spark that makes life feel worth living. It's about metabolic changes that increase risk of diabetes and cardiovascular disease.
These are not vanity concerns. These are quality-of-life issues that deserve the same medical attention and respect as any other hormone deficiency. We don't tell diabetics that insulin is a vanity drug or dismiss thyroid replacement as cosmetic treatment. Why should testosterone be different?
The conflation of legitimate medical TRT with bodybuilding doses of anabolic steroids has done tremendous damage to patient care. Yes, testosterone is sometimes abused for athletic performance enhancement, often at doses far exceeding therapeutic levels. But this doesn't invalidate its legitimate medical use any more than the abuse of prescription painkillers invalidates their role in pain management.
Men with genuine testosterone deficiency deserve evidence-based treatment, not judgment or dismissal. The vanity myth has kept countless men suffering in silence, afraid to even raise the topic with their doctors for fear of being seen as vain or drug-seeking.
When Doctors Treat Numbers Instead of Humans
The flip side of the "normal range" myth is the belief that once testosterone levels are brought into an acceptable range, the job is done, regardless of how the patient actually feels.
This laboratory-focused approach misses the entire point of hormone replacement therapy. The goal isn't to achieve a specific number on a test result. The goal is to alleviate symptoms, improve quality of life, and optimize health while maintaining safety. Laboratory values are important tools for monitoring and adjusting treatment, but they're means to an end, not the end itself.
Some men feel dramatically better when their levels are brought to the mid-range, while others need higher levels to achieve symptom relief. Some men have variations in hormone receptors, binding proteins, or conversion enzymes that affect how they respond to a given testosterone level. Individual variation is the rule, not the exception.
A good TRT protocol involves regular monitoring of not just testosterone, but related markers like estradiol, red blood cell counts, and prostate health indicators. But even more importantly, it involves actually listening to the patient. How's your energy? Your mood? Your cognitive function? Your sexual health? Are you experiencing side effects? These subjective reports are data too, and they're often more clinically meaningful than hitting arbitrary numerical targets.
The numbers-only approach persists because it's easier to follow a protocol than to practice nuanced, individualized care. It's easier to adjust until labs look good and call it success than to engage in ongoing dialogue about symptoms, side effects, and quality of life. But easier isn't better when it comes to hormone optimization.
Moving Beyond Mythology Toward Modern Care
These persistent myths share a common thread: they're rooted in outdated science, oversimplification, and fear rather than current evidence and individualized medicine. They represent a medical approach that treats testosterone as inherently dangerous rather than as a legitimate therapeutic tool requiring appropriate patient selection, monitoring, and management.
The consequences of these myths are real and significant. Men who could benefit from evaluation and treatment avoid seeking help, assuming they'll be dismissed or told their problems are just "part of aging." Men who do seek help encounter doctors who either refuse to consider TRT based on outdated fears or who prescribe it carelessly without proper monitoring. Both extremes are failures of modern medical care.
What men deserve is something in between: thoughtful evaluation of symptoms and lab values, honest discussion of potential benefits and risks, individualized treatment plans when appropriate, and ongoing monitoring and adjustment. They deserve doctors who stay current with evolving evidence rather than practicing based on myths learned decades ago.
The evolution of men's health care has opened new pathways for accessing this kind of informed, patient-centered approach. Platforms like AlphaMD are built around the principle that hormone health requires education, individualization, and careful medical oversight. Rather than either dismissing concerns or taking a one-size-fits-all approach, modern men's health practices emphasize thorough evaluation, transparent discussion of treatment options, and ongoing monitoring to ensure both effectiveness and safety.
TRT isn't right for everyone, and it's not a magic solution to all of life's problems. But for men with genuine testosterone deficiency, it can be genuinely life-changing when done properly. The first step is getting past the myths that have dominated medical thinking for far too long and approaching hormone health with the same evidence-informed, individualized care we expect for any other aspect of medicine.
You don't have to accept feeling half-alive because your doctor is still practicing based on 1941 assumptions or headlines from flawed studies. You deserve evaluation, education, and if appropriate, treatment that's based on where the science actually is in 2026, not where medical mythology says it should be.
Have a question? Ask us.
At AlphaMD, we're here to help. Feel free to ask us any question you would like about TRT, medical weightloss, ED, or other topics related to men's health. Or take a moment to browse through our past questions.
People are asking...
I'm a 36-year-old male, I've been on TRT for hypogonadism for about 10 years now. The TRT specialist/internist I was getting treatment with, emigrate...
We hear a story like yours all the time. GP’s have a lot of things they have to keep up on. New treatments for diabetes, new diagnostics for rheumatic conditions, new screening rules for breast cance... See Full Answer
Age 62, athletic, nutrition freak (usa). Started TRT 15 months ago when testosterone at 298. Six months later it was 498 and I was doing great. Level ...
I'll share some conjecture here without knowing more. Taking everything at face value, I would say whatever medication you're taking might not be Testosterone Cypionate. When you take any Testosterone... See Full Answer
Hi, I’m 25 years old. Test is 404. I work out 5 days per week, am pretty lean and fit and healthy I had previously considered TRT but ultimately turn...
A few things to note: You may have relative hypogonadism where your numbers just being low aren't the main factor to determine treatment. 400 would be within that range. You will lose Testosterone ove... See Full Answer
Get $30 off your first month’s order
Enter your email address now to receive $30 off your first month’s cost, other discounts, and additional information about TRT.
Legal Disclaimer
This website is a repository of publicly available information and is not intended to form a physician-patient relationship with any individual. The content of this website is for informational purposes only. The information presented on this website is not intended to take the place of your personal physician's advice and is not intended to diagnose, treat, cure, or prevent any disease. Discuss this information with your own physician or healthcare provider to determine what is right for you. All information is intended for your general knowledge only and is not a substitute for medical advice or treatment for specific medical conditions. The information contained herein is presented in summary form only and intended to provide broad consumer understanding and knowledge. The information should not be considered complete and should not be used in place of a visit, phone or telemedicine call, consultation or advice of your physician or other healthcare provider. Only a qualified physician in your state can determine if you qualify for and should undertake treatment.
